Dr Cinzia Papadia MD FRCP, consultant gastroenterologist at Barts Health NHS Trust and honorary senior lecturer at Queen Mary University of London
Dr Cinzia Papadia MD FRCP – consultant gastroenterologist at Barts Health NHS Trust and honorary senior lecturer at Queen Mary University of London – recently led a study of the performance of BIOHIT HealthCare’s GastroPanel® in the identification of moderate to severe atrophic gastritis (AG) – a common precursor to gastric cancer – in dyspeptic patients. This blog provides an overview of the key findings and conclusions from this paper, which has now been published in BMJ Open Gastroenterology. It also explores the potential of routine clinical GastroPanel use to streamline current diagnostic pathways and improve access to urgent endoscopy procedures for those most at risk.
Gastric cancer is a significant global health burden, ranking as the sixth most common cancer worldwide, with an age-standardised incidence rate of 11.1. In the UK, gastric cancer is the 17th most common cancer, accounting for 6,568 new cases annually, with only 22 per cent of patients surviving beyond five years. Alarmingly, over half (54 per cent) of these cases are considered preventable, yet late diagnosis remains a major hurdle to improving outcomes.1–6 Early diagnosis has been shown to significantly improve survival rates, as evidenced by successful screening programmes in countries like Japan and Korea. These initiatives have achieved earlier detection of AG and subsequently better prognoses. In contrast, the UK, US and Europe lack routine screening schemes for gastric cancer, and rising cases in younger populations have sparked discussions at the European Council on the need for prevention strategies.
AG is the most common environmental pre-neoplastic condition for gastric cancer, with its severity directly linked to cancer risk. Studies have shown that moderate to severe AG increases the risk of gastric cancer up to 90-fold.7,8 Other risk factors include lifestyle behaviours – such as high salt intake, alcohol misuse and unhealthy diets – as well as Helicobacter pylori (H. pylori) infection and autoimmune AG.9 Despite these known risk factors, limited patient stratification based on individual risk, including family history and smoking habits, further hinders early diagnosis efforts. Currently, identifying AG as the root cause of dyspepsia relies heavily on endoscopy, but its usefulness in those with more minor or non-specific dyspeptic symptoms is limited. Moreover, endoscopy is invasive, resource intensive and constrained by delays and long waiting lists. Endoscopic evaluation also suffers from variability between clinicians, complicating consistent and early identification. These challenges highlight the need for an effective, non-invasive triage tool to identify patients at high risk for AG and gastric cancer, while sparing unnecessary procedures in low risk patients.
Transforming gastric diagnostics with biomarker-based approaches
Biomarker-based detection methods, such as GastroPanel, present a promising solution. GastroPanel is a non-invasive diagnostic kit which tests for specific AG biomarkers – pepsinogen I (PGI), pepsinogen II (PGII), their ratio (PGI/PGII), gastrin-17 (G-17) and H. pylori IgG – that can be used in combination to quickly and accurately detect stomach pathologies like moderate to severe AG.10 These specific biomarkers provide a comprehensive view of stomach mucosa function, with PGI and PGII reflecting corpus integrity, and G-17 indicating antral mucosal health and acid production.11–13 A lower PGI/PGII ratio and elevated gastrin levels, particularly in the absence of H. pylori antibodies, are indicative of advanced atrophic changes.14,15 The integration of non-invasive, biomarker-driven tools such as GastroPanel into clinical practice therefore offers the potential to revolutionise gastric cancer prevention, improving early detection and reducing reliance on invasive diagnostics.
Validating GastroPanel as a triage tool
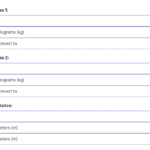
A single-centre prospective diagnostic accuracy study was conducted between February 2017 and January 2019 in the Gastroenterology Department of Homerton University Hospital, London. It included 324 dyspeptic patients who had been referred for gastroscopy without alarm symptoms in line with UK dyspepsia pathway guidelines. Each participant provided fasting blood samples for analysis using the GastroPanel ELISA test, with results classified into diagnostic categories by the GastroSoft™ software. Gastroscopy and biopsies were performed by experienced endoscopists, with samples processed and analysed for H. pylori infection, AG, gastric intestinal metaplasia and dysplasia by expert histopathologists, blinded to GastroPanel results. Key metrics like sensitivity, specificity and predictive values were calculated for GastroPanel biomarkers.
The study demonstrated strong agreement (90 per cent, κw: 0.828) between GastroPanel and histology for detecting moderate to severe AG. Biomarker analysis showed the PGI/PGII ratio (cut-off 3.0 μg/l) had an AUC of 0.960 – with 75 per cent sensitivity and 98 per cent specificity – while PGI (cut-off 25 μg/l) achieved an AUC of 0.840, with 75 per cent sensitivity and 99 per cent specificity. Positive GastroPanel results indicated an 86 per cent probability of moderate/severe AG, while negative results had a 1 per cent post-test probability. These findings highlight GastroPanel’s precision in identifying moderate to severe AG and its potential to improve diagnostic pathways by reducing unnecessary endoscopies and guiding targeted patient care.
Advantages for gastric cancer detection and management
This study gives further evidence showing that GastroPanel offers significant advantages for the detection and management of precancerous conditions, and aligns with the 2019 British Society of Gastroenterology guidelines advocating early detection through non-invasive testing prior to endoscopy. The test can be used as a first-line assay in primary care, helping to triage dyspeptic patients without alarm symptoms at the point of care. GastroPanel also supports improved risk stratification by integrating results with clinical risk scores, enabling healthcare professionals to enhance predictive accuracy and prioritise patients for timely intervention. The test’s high sensitivity and specificity in detecting moderate to severe AG address challenges associated with variability in histological assessments, and support the effective distinction of functional dyspepsia and high risk AG cases. Additionally, results can guide further diagnostic procedures, such as targeted endoscopies and narrow-band imaging, further improving diagnostic efficiency and patient outcomes.
Another particular strength of GastroPanel is its non-invasive nature, which also reduces the need for repeated endoscopies and improves the patient experience. Reducing unnecessary endoscopies greatly streamlines diagnostic pathways and ensures resources are focused on patients most in need.
Minimising unnecessary procedures and their associated risks could also lead to significant savings for the NHS annually.
Emerging areas of research and application
Dr Papadia’s study demonstrates that GastroPanel could be a promising step towards improving early detection and management of precancerous gastric conditions, enhancing patient outcomes and alleviating strain on healthcare resources. GastroPanel offers precision in identifying atrophic and autoimmune gastritis through biomarkers like pepsinogen I, pepsinogen II and gastrin-17 and, in doing so, it addresses critical gaps in current diagnostic pathways. Its quick test format further streamlines diagnostics in primary care and bedside settings, reducing laboratory delays and improving accessibility. Future research should focus on its application in triaging dyspeptic patients without alarm symptoms, as well as its potential in reducing the burden on overextended endoscopy services. Additionally, its role in monitoring patients with histologically and serologically assessed gastric atrophy, along with its economic and environmental impact, warrants further exploration. However, mounting evidence, such as that from the recent London GastroPanel study, already makes a strong case for integrating GastroPanel into clinical pathways as a practical, non-invasive and cost-effective solution for the early detection and management of gastric cancer.
References
- Rachael Harker. Cancer Statistics for England.; 2024. Accessed January 20, 2025.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249. doi:10.3322/caac.21660
- HOWSON CP, HIYAMA T, WYNDER EL. THE DECLINE IN GASTRIC CANCER: EPIDEMIOLOGY OF AN UNPLANNED TRIUMPH. Epidemiol Rev. 1986;8(1):1-27. doi:10.1093/oxfordjournals.epirev.a036288
- Correa P, Haenszel W, Cuello C, et al. Gastric Precancerous Process in a High Risk Population: Cohort Follow-up1. Cancer Res. 1990;50(15):4737-4740.
- Plummer M, Franceschi S, Muñoz N. Epidemiology of gastric cancer. IARC Sci Publ. 2004;(157):311—326.
- Hu B, El Hajj N, Sittler S, Lammert N, Barnes R, Meloni-Ehrig A. Gastric cancer: Classification, histology and application of molecular pathology. J Gastrointest Oncol. 2012;3(3).
- Sipponen P, Maaroos HI. Chronic gastritis. Scand J Gastroenterol. 2015;50(6):657-667. doi:10.3109/00365521.2015.1019918
- Nordenstedt H, Graham DY, Kramer JR, et al. Helicobacter pylori -Negative Gastritis: Prevalence and Risk Factors. American Journal of Gastroenterology. 2013;108(1):65-71. doi:10.1038/ajg.2012.372
- International Agency for Research on Cancer. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Schistosomes, Liver Flukes and Helicobacter Pylori. Vol 61. National Institute of Health, National Center for Biotechnology Information; 1994.
- NARDONE G, ROCCO A, STAIBANO S, et al. Diagnostic accuracy of the serum profile of gastric mucosa in relation to histological and morphometric diagnosis of atrophy. Aliment Pharmacol Ther. 2005;22(11-12):1139-1146. doi:10.1111/j.1365-2036.2005.02734.x
- Agréus L, Kuipers EJ, Kupcinskas L, et al. Rationale in diagnosis and screening of atrophic gastritis with stomach-specific plasma biomarkers. Scand J Gastroenterol. 2012;47(2):136-147. doi:10.3109/00365521.2011.645501
- Biohit Oyj. GastroPanel®, Forms and instructions.
- Väänänen H, Vauhkonen M, Helske T, et al. Non-endoscopic diagnosis of atrophic gastritis with a blood test. Correlation between gastric histology and serum levels of gastrin-17 and pepsinogen I. Eur J Gastroenterol Hepatol. 2003;15(8):885-891. doi:10.1097/00042737-200308000-00009
- SYRJÄNEN K. Accuracy of Serum Biomarker Panel (GastroPanel ® ) in the Diagnosis of Atrophic Gastritis of the Corpus. Systematic Review and Meta-analysis. Anticancer Res. 2022;42(4):1679-1696. doi:10.21873/anticanres.15645
- Lansdorp-Vogelaar I, Kuipers EJ. Screening for gastric cancer in Western countries. Gut. 2016;65(4):543-544. doi:10.1136/gutjnl-2015-310356